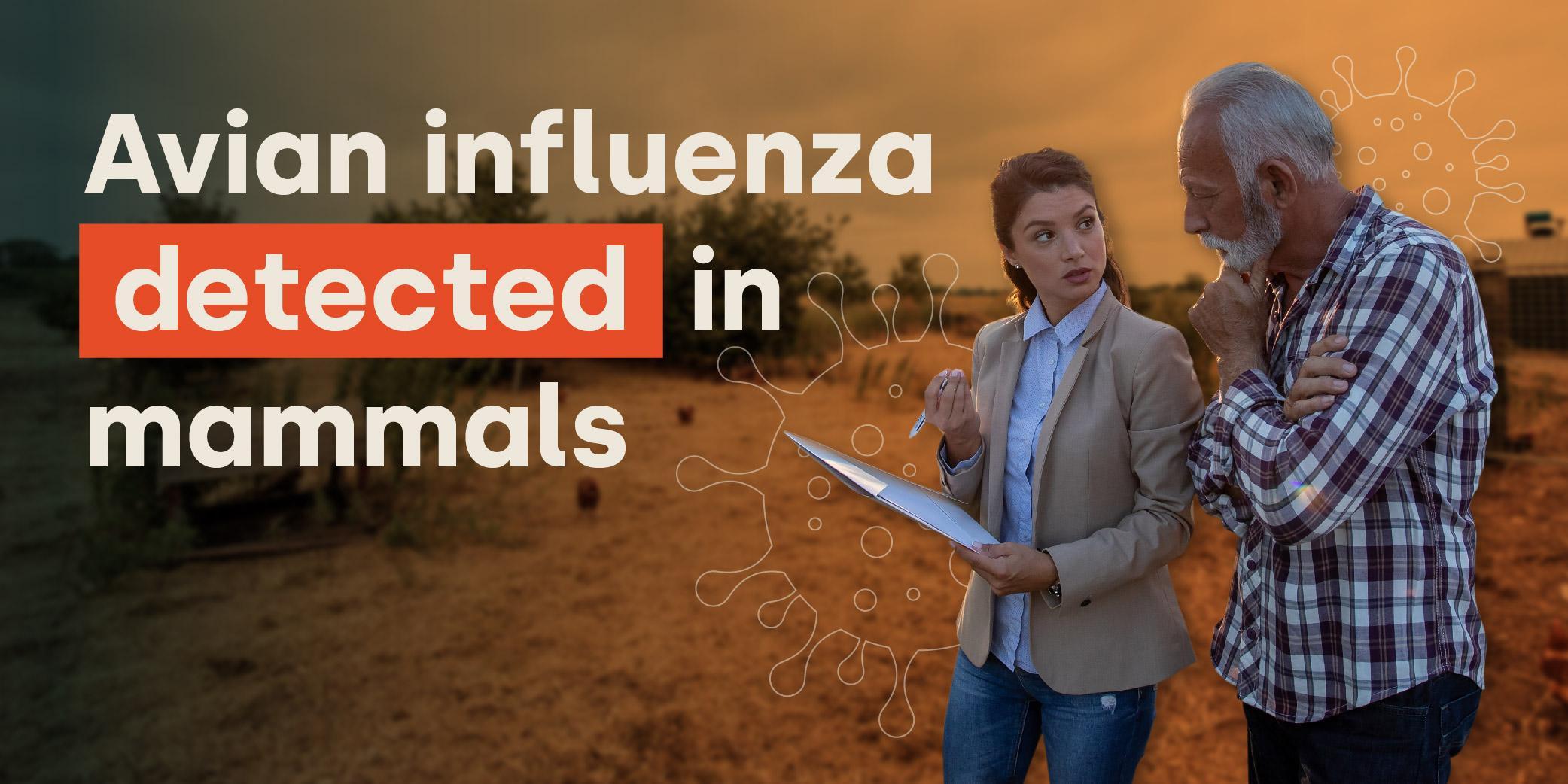
Highly pathogenic avian influenza H5N1 has spilled over into mammals.
Over the last 18 months the World Organisation for Animal Health (WOAH) has had reports that non-avian species have been affected by the virus. Internationally, H5N1 has been recorded in grizzly bears, racoons, mink, leopards, seals and dolphins. Most recently in the UK it has also been confirmed in a small number of otters and foxes.
The Animal and Plant Health Agency (APHA) Director of Scientific Services, Professor Ian Brown, explained that if a scavenging mammal eats a dead or sick bird, they would be exposed to “very large quantities of virus”. He goes on to say that this opens up the possibility for the virus to enter a new host population which it is not normally found in.
Whilst at present there is no evidence that a fox or otter could transmit the disease to another of its species, it is imperative that action through enhanced biosecurity is taken to ensure that the spread of the deadly disease is minimised in the wild and captive mammal population.
Should we be worried?
Incident director, Dr Meera Chand at the UK Health Security Agency (UKHSA), has said that “Latest evidence suggests that the avian influenza virus currently circulating in birds does not spread easily to people”.
International health agencies however, have expressed concern that the spillover into mammals represents a change in the epidemiology of the virus. The UKHSA do also express the need to practise caution, warning that due to the mutations in the virus found in mammals, the virus “has a propensity to cause zoonotic infections”, meaning the potential ability to infect humans.
It is important to note that H5N1 has been confirmed in people within the past 20 years. The World Health Organisation (WHO) has recorded almost 870 cases in humans, leading to 457 fatalities. Most recently, there have been five human cases confirmed since September 2021, with one in the UK and another causing a fatality in China.
What is the Government doing about it?
Professor Jones of The Department for Environment, Food and Rural Affairs (Defra) has said that the department and the devolved administrations are working together in an active programme for detecting the virus in scavenging mammals that might feed on wild birds. This data will be shared with public health authorities.
The UKHSA is also looking at new ways to test humans who work with poultry and have been exposed to the disease, but who may be asymptomatic.
APHA and UKHSA are on alert and are “watchful” and remain “vigilant for any evidence of changing risk.”
Symptoms of bird flu in people
People who have come into contact with those who care for poultry, which have been confirmed as infected, should monitor their health. They should do the same if they know they have been in contact with an animal that has also been associated with dead poultry or wild birds. In these instances they should look for symptoms of infection for 10 days after their exposure. Symptoms of H5N1 in humans to check for include:
- Trouble breathing or a shortness of breath
- An itchy cough
- Sore throat
- Running or stuffy nose
- Eye irritation, such as redness and weeping
- Headaches
- Muscle aches
- Diarrhoea
Serious cases in mammals
In March 2023 in post mortem samples, ten South American bush dogs were found to be positive for highly pathogenic avian influenza (H5N1). They were part of a captive breeding programme at a zoo in England.
Other serious cases of H5N1 in mammals recently include 50,000 mink on a farm in Spain, which prompted the need for emergency depopulation to stop any further spread. Mink are known to be susceptible to a number of human respiratory diseases.
Avian influenza H5N1 was also found in roughly 700 dead seals that died in what is coined a ‘mass mortality event’ in the Caspian Sea.
How can Livetec help protect your workers?
With avian influenza firmly rooted on UK shores and its mutation enabling it to infect mammals, good on-farm biosecurity is vital.
Not only does a comprehensive biosecurity plan provide high animal welfare and protect your business, but it guards your workers, visitors and any pets from the potential risk of transmission.
Livetec have been building the future of biosecurity for over a decade. Our evidence-based plans are designed to protect livestock and the people who care for them.
Biosecurity should be embedded into the day-to-day operation of a farm business. To find out more about how Livetec can help contact one of our Biosecurity Advisers here.